The Geriatric Emergency Department Intervention (GEDI) focusses on the frail older person presenting to an Emergency Department (ED) with an acute illness or complex healthcare requirements. Usually this incorporates people of 75 years of age and over. However, frail older persons who are under this age and Indigenous Australians 55 years of age or older, who may have similar levels of frailty, are also screened by the team and may be included in service delivery. The GEDI model is aimed at improving the quality of care for this cohort, reducing unnecessary hospital admissions and facilitating early safe discharge. The GEDI team consists of an ED physician champion with a special interest in aged care and Clinical Nurses (CNs) led by a Clinical Nurse Consultant (CNC). The CNC implements policy and procedures underpinning the GEDI model, manages the nursing team, provides clinical expertise and leadership, provides education to all ED staff and builds a culture within the ED that values and prioritises person-centred care of frail older persons.
The GEDI service may absorb, replace or collaborate with a range of other services provided for frail older people in the ED. For example, the Community Health Interface Program (CHIP) that operates in many Queensland EDs and supports referral of clients to community-based nursing and allied health resources may be enfolded into the GEDI model. Because GEDI is a service managed within the ED it can be responsive to the needs and timelines of ED and facilitate appropriate referral and discharge planning. However, the GEDI model fundamentally incorporates a ‘border spanning’ role aimed at improving inter-disciplinary communication, entrenching patient-centred decision making, facilitating safe hospital discharge where possible and improving fast-tracking of referral and admission processes when required.
Underpinning principles of the GEDI model
The GEDI model and the nurse-led approach to this model are underpinned by a number of theoretical frameworks. These are: Integration of health service delivery (World Health Organisation (WHO), 2008), Recognition primed decision making theory (Klein, 1998), the Shared decision making framework (Frosch & Kaplan, 1999), Nursing role effectiveness model, the integrated – Promoting Action on Research Implementation in Health Services (i-PARIHS) framework (Harvey & Kitson, 2016), Diffusion of innovations, in particular champions of change (Rogers, 2003) and national and international guidelines. The GEDI model seeks to integrate health service delivery within the hospital and between sectors (WHO, 2008). The GEDI nurses undertake their assessment, clinical decision making and interventions using a recognition primed decision-making approach (Klein, 1998) with a focus on shared decision making (Frosch & Kaplan, 1999). The functioning of the GEDI team incorporates the GEDI physician being a champion of change while the advanced practice nurses incorporate largely interdependent and independent roles (Doran, Sidani, Keatings, & Doidge, 2002). These principles and frameworks will be referred to throughout the document and a short explanation is provided here.
Improving outcomes for older persons in the ED requires an integrated system of health service delivery. The World Health Organisation (2008) proposes that integrated care provides people with the care they need, when they need it, in ways that are user friendly, achieve the desired results and provide value for money. For frail older persons, presentation to the ED may be as a result of a critical event marking a drop in functional decline or may be due to difficulty accessing primary care.
Types of integration
- Linkage: links are established between the most appropriate health services to ensure the best possible health outcomes for all clients
- Coordination: integrating services to fill gaps in service provision, therefore working across sectors
- Full integration: one set of management support systems supporting the whole service
Levels of integration
- System integration: the services are provided within one unified system
- Organisational integration: services are provided by linking different organisations within a system
- Clinical integration: services are provided through the integration of different clinical services within a system or organisation
Forms of integration
- Vertical integration: different levels of service under one management system for referring patients up and down appropriate levels. Each service addresses a specific healthcare issue and clear objectives
- Horizontal integration: consolidating organisations that provide a similar level of healthcare under one management umbrella, therefore sharing resources to increase efficiency
The provision of a fully integrated service for older persons moving between two or three sectors (i.e. aged care, primary care and secondary care) when these parts of the system are funded differently and have different performance indicators, is a challenge yet to be successfully addressed in Australia. The GEDI nurses do not provide a fully integrated service but rather ensure linkage between the different sectors and through expert communication provide improved co-ordination of service delivery. They are largely able to facilitate organisational and clinical integration in a horizontal manner increasing the efficiency of care management within the hospital.
A key point of difference between the depth of advanced practice of GEDI nurses and the breadth of practice of ED primary nurses is in their use of recognition primed decision making (Klein, 1998). This is an approach to decision making in which the expertise of the GEDI nurses, and their dual preparation in both emergency and gerontological care, provide them with a series of internal working models (based on experience and knowledge) that allow them to streamline and fast-track complex decision making around this vulnerable group.
Shared decision making in the ED is a method of actively engaging patients, their families or carers to reach mutual agreement with clinicians in decisions that directly affect their health (Charles, Gafni & Whelan, 1997). This differs from informed consent which focuses on one medically superior option (Frosch & Kaplan, 1999). In shared decision making, there are at least two medically reasonable options and the decision relies on patient values and preferences (Probst, Kanzaria, Schoenfeld, Menchine, Breslin, Walsh…Hess, 2017). This is a focus in the GEDI model where the GEDI nurse gathers information from many sources including the patient, family or carer, to influence medical disposition planning.
With reference to the Nursing Role Effectiveness Model developed by Doran and colleagues (2002), the GEDI nurses predominantly perform independent and inter-dependent roles. This is important because without the ability to influence key medical decision making and to instigate diagnostic testing, intervention and direct referral to specialist medical and allied health professionals, diagnosis and disposition management can become stalled. Due to their independence and ability to facilitate multidisciplinary discussion and decision-making, the care of vulnerable, frail, older persons in the ED can be streamlined and fast-tracked.
The i-PARIHS knowledge translation approach aims to facilitate knowledge translation (Harvey & Kitson, 2016). It is suggested that settings wishing to implement the GEDI model of service delivery base their SCHHS GEDI approach on i-PARIHS and a Cochrane review that provides evidence of the importance of tailoring interventions to the context (Baker, Camosso-Stefinovic, Gillies, Shaw, Cheater, Flottorp, … Jäger, 2015). In this approach, there are two layers of facilitators: external facilitators who will support all participating sites and an internal (hospital-based) facilitator who will be the local champion. The ED physician champion and the ED CNC from a well-established GEDI service centre are the external facilitators and the internal facilitators are the appointed ED physician champion and the GEDI CNC at the implementation site.
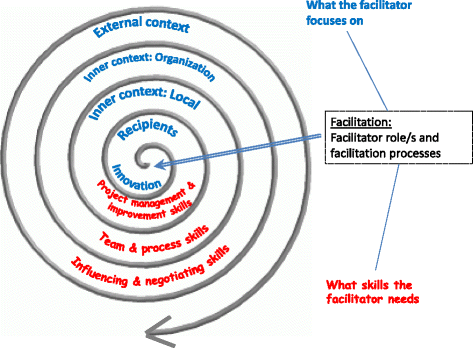
According to i-PARIHS, the external facilitator is a knowledge broker, linking the knowledge producers (i.e. clinical and research team) to the recipients or knowledge users (i.e. hospital ED staff). These people have skills in knowledge translation, change management, negotiation and influence, and their activities will include mentoring, coaching and guiding the internal facilitators. They have also developed resources related to facilitation for a web-based toolkit, to train and develop a support network for the other facilitators where ‘tricks of the trade’ will be shared. Their support includes a face-to-face visit, regular teleconferences and moderating cyber forums, where facilitators will discuss issues.
The internal facilitators (ED physician and GEDI CNC) reflect the role of boundary spanners in i-PARIHS, whereby they interact and connect with local staff and the external facilitator. The internal facilitators bring content expertise related to care of older persons in the ED, contextual knowledge of the hospital system and how to navigate hospital processes. They will receive guidance from the external facilitator to develop and apply skills in knowledge translation and change management. Internal facilitator activities include assisting in ward planning meetings, helping the local staff undertake environmental scans, supporting the development of action plans, and guiding local staff to implement the plans. They will present the toolkit to staff and establish a local support program, enabling local staff to share their knowledge about what works and doesn’t work in the local context.
The internal facilitators are the local context experts and understand the recipients (i.e. local ED staff). They will lead ED staff and management team meetings during which first an environmental scan is undertaken and then an action plan targeting strategies to maximise enablers and overcome barriers to implementing the GEDI model is developed, guided by a structured framework (Harvey & Kitson, 2016). These plans will address factors in their immediate and wider contextual environments that act as enablers or barriers to the delivery of the GEDI service. ED staff, the external and internal facilitators will contribute to these plans. Internal facilitators, with support of the external facilitator, will lead the enactment of this plan and monitor its progress.
The role of the ED physician in the GEDI team is primarily a champion for organisational change. This enables the innovation to be embedded into the ED and creates the environment for ongoing sustainability of change. The Diffusion of Innovations theory postulates that champions advocate for change and need influence within an organisation to succeed (Rogers, 2003). They require energy, creativity, skills in negotiation with all levels and are key to continuing to overcome barriers, influencing new management and executive staff to understand the innovation and sustainability requirements (O’Loughlin, Renaud, Richard, Gomez & Paradis, 1998). Importantly, champions share the ambitions of the recipients of change, in the case of the GEDI model, the needs of the older person in the ED, they balance the diverse needs of groups and embody strategic leadership (Rogers, 2003; Batras, Duff & Smith, 2016). This role is crucial to the success of the GEDI service.
This toolkit references a variety of national and international guidelines that focus on geriatric emergency care. More information about care of older persons in the ED can be found in the following documents:
Objectives of the GEDI model
The objectives of the GEDI model are to:
- Maximise patient-centred multidisciplinary decision making for frail older persons in the ED
- Identify the goals of presentation that are important to the patient and/or carers
- Fast track patient assessment and multidisciplinary decision-making
- Identify functional decline
- Reduce morbidity
- Increase appropriately supported safe discharge from the ED
- Reduce avoidable admissions to hospital
- Reduce hospital length of stay
- Reduce avoidable re-presentations to the ED
Attention
The GEDI model is an innovation, provided in a consultant capacity, focussing on early assessment of frail older patients, aimed at clinical and disposition decision making.
The patient journey
The journey of a typical frail older person from a residential aged care facility (RACF) with complex needs through the ED with and without the support of the GEDI service. The patient journey's are provided to emphasise the potential areas of impact that GEDI may have.
Benefits of the GEDI model
The benefits of the GEDI model include:
Fast tracking
- Early identification through the iEMR/EDIS system or a phone call from RACF/QAS
- Prioritisation of patients referred to and seen by GEDI nurses
- Early geriatric screening by GEDI nurses utilising the clinical frailty score (CFS) identifies people with complex care needs enabling timely, goal centred care
- Rapid assessment and targeted care whilst in ED
Improved patient care
- Rapid and targeted assessment of physical and cognitive functioning (e.g. delirium screening)
- Access to wide range of information from patient, medical records, RACF/GP/family/carers
- Formulates patient issues and goals of treatment – discusses with family and carer
- Early initiation of independent nursing interventions as required (e.g. replacement of IDC, wound management)
- Facilitates and communicates combined progress planning
Improved care coordination with medical and allied health professionals
- Coordination of care within the ED to achieve goals of treatment
- Coordinates additional assessment by specialist medical or allied health professionals
- Liaises with bed manager, medical team and primary nurse
- Direct referral to specialist medical or allied health professionals
Facilitation of care
- Influences range and scope of diagnostic testing
- Coordinates chronic disease management and further treatment
- Influences disposition course
Reduce need for patient hospital admission
- Liaises with and organises community support to facilitate requirements for discharge
- Provides targeted assessment and care for geriatrics in ED – ability for patients to obtain further assessment or care during 24 hour stay in a ward in the ED such as a Short Stay Unit (SSU) to support discharge home without prolonged admission to hospital ward
- Organises follow up through required medical/support services
- Provides medication script and medications if required to facilitate ongoing care and ensure current planned care may be followed.